Achondroplasia is a rare, genetic condition that affects bone growth. It is the most common type of skeletal dysplasia. Achondroplasia causes bone growth to slow down, especially in the long bones of the arms and legs. This causes short stature, shortened limbs, and other distinctive features.1
Definitions of key terms can be found in the glossary

Achondroplasia is caused by variants in the fibroblast growth factor receptor 3 (FGFR3) gene. FGFR3 plays a key role in regulating bone growth.1,2
Achondroplasia occurs in about 1 in 25,000 births. The variants that cause achondroplasia can occur either by chance or from being passed down by a parent with the condition.1
Most of the time, the variant occurs in families with no prior history of achondroplasia. In families where one parent has the condition, there is a 50% chance that the variant will be passed down to the child.1
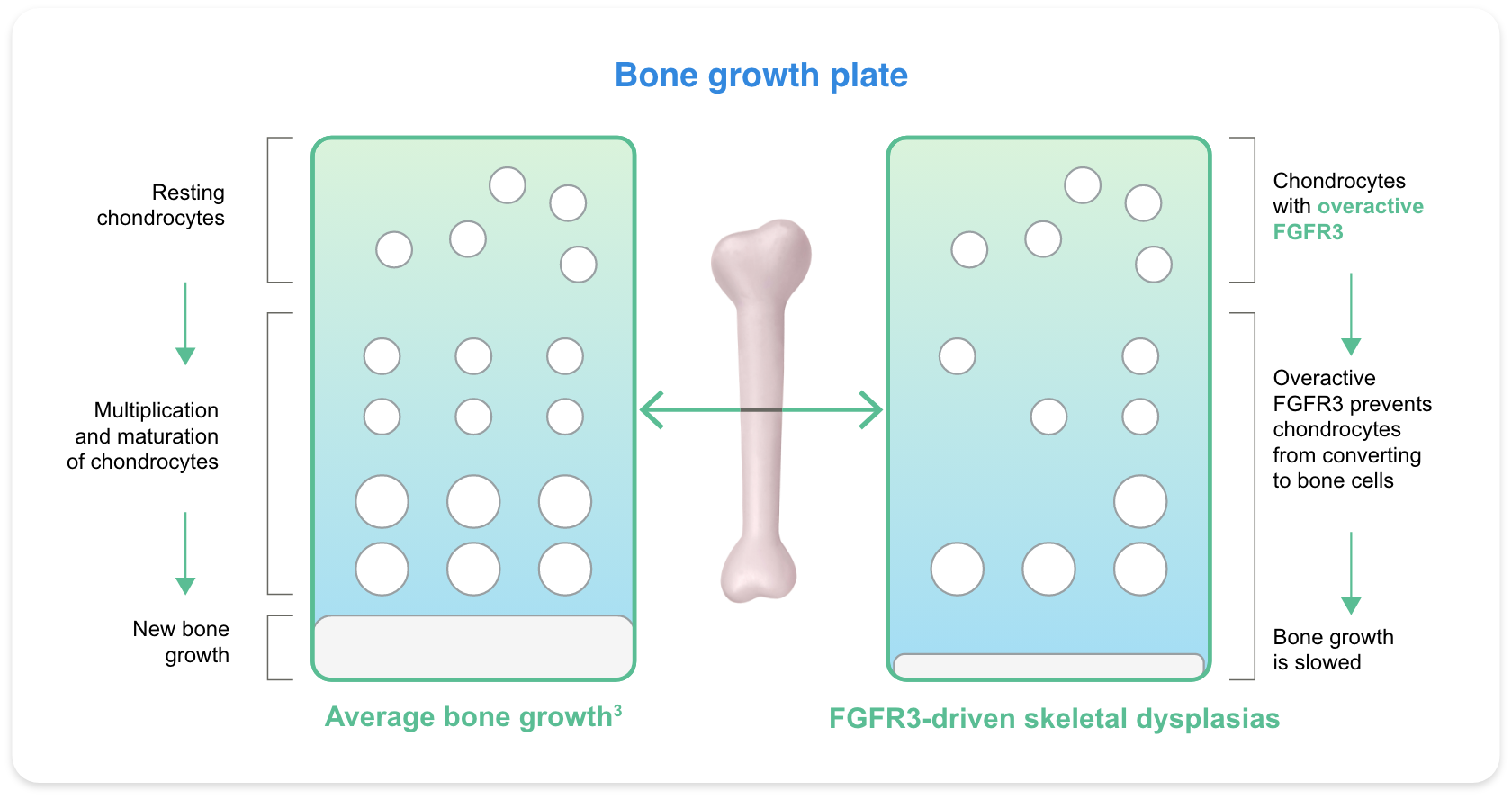
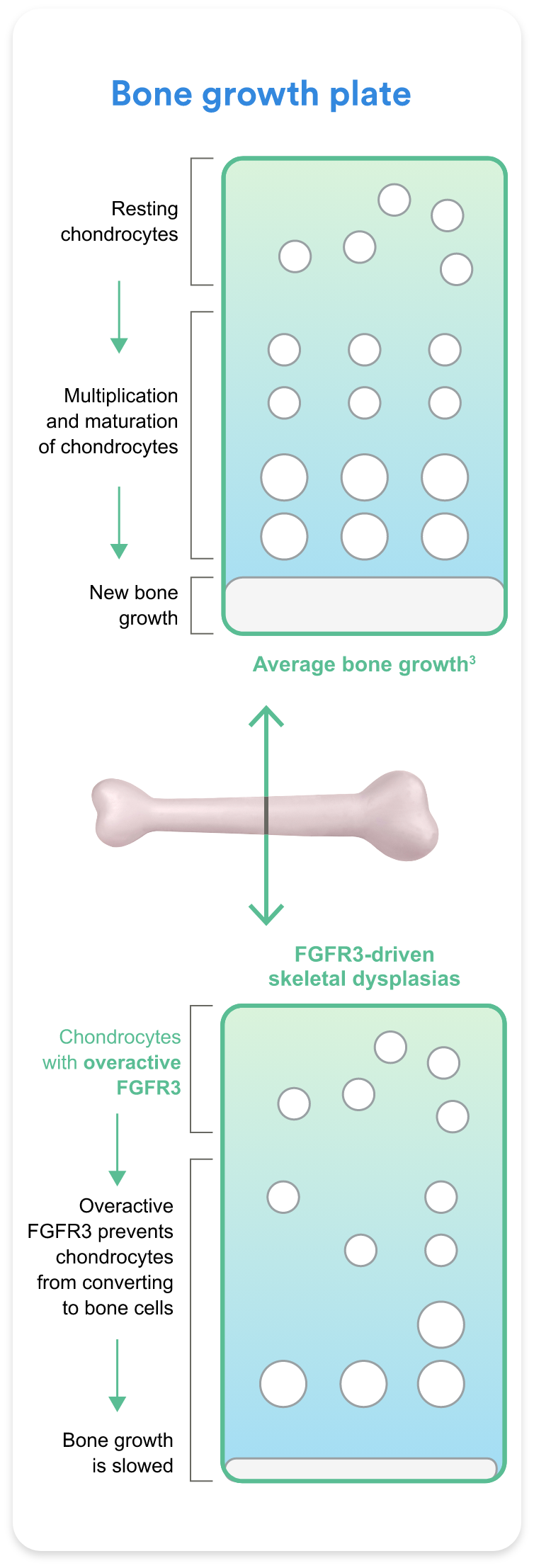
Chondrocytes are a type of cell responsible for bone and cartilage formation. They are essential for the development of the skeletal system.2,3
Chondrocytes contain a type of protein called FGFR3, which helps to slow bone growth.2,3
In people with achondroplasia, FGFR3 becomes overactive, which reduces bone growth and leads to the common features of achondroplasia.1
 Enlarge image
Enlarge image
The way bones grow in people with achondroplasia can lead to specific medical complications and challenges. Multiple systems in the body can be affected and symptoms may vary at different stages of life.4-6 Achondroplasia complications that may occur are shown in the table below.
Individuals with achondroplasia should have regular check-ups by an experienced, multidisciplinary healthcare team. Some complications may improve on their own, while others may require treatment or surgery. Some children may benefit from early intervention.6 Learning about the complications that may occur can help individuals and families feel prepared and get the care needed.
Talk to a member of your healthcare team
for guidance on your care plan



Infancy
Childhood
Adolescence
Adulthood
Slowed or repeated stopping of breathing during sleep
Crowded or crooked teeth, narrow palate, open bite or underbite
May lead to delayed speech or hearing loss
Upper airway obstructions
Poor muscle tone
Narrowing of the opening at the base of
the skull, which can affect breathing or develop into other complications
Narrowing of the lower spinal cord, which may cause pain and other complications
Outward curving (rounding)
of the upper back
Inward curving (arching) of the lower back
Bowed legs
Widespread joint and muscle pain
Obesity
Infancy
Childhood
Adolescence
Adulthood
Definitions of these terms can be found in the glossary
People with achondroplasia generally live healthy, active, and independent lives. However, some activities can be challenging due to the way that bones develop in achondroplasia.5
Learning about adaptations and options for support can enhance independence and well-being
Quality of life
The experience of living with achondroplasia is different for each individual and each family. Many factors, such as functional limitations, social stigma, or emotions, can affect quality of life.7-9
Adaptations and tools, such as step stools and personal care devices, can support independence in daily activities.1 Psychological support from healthcare professionals as well as social support from family members, peers, and advocacy groups may enhance well-being.4,6